On Friday, an international teleconference at Eastern Michigan University addressed several aspects of gerontology and health care facing older adults in room 108 of the Marshall Building. The conference included multiple fields and was broadcasted live to 5,000 medical personnel from 32 hospitals in Ukraine alone.
Through the use of Microsoft Link, Russian and Kazakhstani medical professionals were also in attendance, totaling to 5,000 participants. Those in attendance were privileged to seven presentations spanning multiple disciplines.
The conference was hosted by EMU’s David W. Thomas. Thomas is a professor in the School of Health Sciences and director for the Therapeutic Recreation Program on campus. A panel of six faculty members gave presentations on various subjects concerning health care for older adults.
The teleconference involved perspectives from the U.S. and Ukraine. It began with Ukraine discussing problems they see in aging veterans and the population as a whole aging at acceleration. A presentation on accelerated aging was given by Dr. Vladislav Bezrukov, director of the Institute of Gerontology and head of the Ukrainian Society of Gerontology and Geriatrics.
“The affiliation with Ukraine’s Institute of Gerontology has been developed over the last nine years when I begin researching dementia care hospitals in 2004 in eastern Ukraine,” Thomas said. “This eventually led to contacts with the director of the Medical Academy of Post Graduate Education and the Institute of Gerontology in Kiev along with contacts in Donetsk and other areas in eastern Ukraine.”
“National Trends in Social Work Practice with Aging Populations” was presented by Deanna M. Miller. Miller is a social worker for Jackson County Medical Care and part-time lecturer at EMU. Miller presented many statistics of interest not only to the aging community, but to each U.S. citizen, as the concerns in health care are growing.
Miller stated that although many nations are facing similar increases in the older population, specifically over the age of 65, the U.S. is struggling to handle this steady rise. According to the Administration on Aging, 19 percent of the population in 2030 will be represented by those ages 65 and older. This is due to the “baby boom” generation that arose post-World War II.
Miller discussed the benefits of Medicare and Medicaid in the U.S., but also how social security and pension benefits may be at risk. Today’s elderly also do not save like previous generations did.
Another topic that Miller hit during her presentation involved the lack of benefits for elderly LGBT couples. In the states where marriage is not legal for them, partners are unable to receive benefits and are not eligible for social security. Also, many LGBT elderly hesitate to seek care, in nursing homes for example, due to fear of discrimination. The proportion of minority elderly will increase over the years as well. According to Miller, we should be “embracing diversity.”
“Acute Care for Elders (ACE) Unit: An Overview,” presented by EMU nursing professor Dr. Virginia M. Lan, discussed the program that was originally developed in 1994 by Dr. Seth Landefeld at University Hospitals Case Medical Center in Ohio.
ACE is one of a few programs designed for acutely ill persons in the age group of 65 and older.
These medical care units focus on early rehabilitation, discharge planning and prepared or modified environments to promote functioning. Lan explained that in these facilities there is patient-centered care and the area is “spacious and private.” Family and friends are encouraged to visit with no limiting hours. There is a local ACE unit at St. Joseph Mercy Hospital in Ann Arbor, Mich.
“Balance Assessment and Movement Programs for Older Adults” was presented by Dr. Phillip Bogle, a professor of exercise and sport science. His presentation stressed the issue concerning balance in older adults, as well as specific screening assessment procedures. According to Bogle’s presentation, medical costs associated with falls in older adults totaled $30 billion in 2010. An issue with older adults is loss of fitness, which increases their risk of falling.
“Even though we age, there is a great deal of plasticity that can be challenged,” said Bogle.
In the U.S., 1 out of 3 older adults aged 65 and older falls each year, but less than 50 percent of those adults speak with a physician concerning the situation. Falls are the leading cause of fatal injuries in older adults, and the rate has increased over the last 10 years. Those who fall often develop a “fear of falling,” which leads to decreased activity and in turn reduces physical fitness, which can increase the chances of another fall.
“Omega-3 Polyunsaturated Fatty Acids (PUFA), Bone Health and Frailty in Postmenopausal Women” by Dr. Heather Hutchins-Wiese stresses the goal of osteoporosis management as reducing the risk of future bone fractures among the older adult community. According to her presentation, the cost of bone fractures in the U.S currently stands at $14 billion.
Hutchins-Wiese, an EMU faculty member, presented findings on the relationship between diet, nutrition and the overall health of the older community. Findings show increases in walking speeds of those older adults administered LC n-3 PUFA compared to the placebo group, although it was stated in the presentation that the dose may not have been high enough to show the true impact on bone turnover.
“Affordable Health Care Act and its Impact on Long-Term Care,” presented by EMU program director for health administration, Dr. Pamela Walsh, discussed the types of long-term care available in the U.S for the older population including nursing facilities, assisted living facilities, community-based services and care available in the home setting. The average cost of a semi-private nursing home in the U.S is $6,235 a month or a total of $205 a day.
The average cost for LTC services in 2012 was 15 percent out of pocket, despite health care. The main points of the Affordable Health Care Act were addressed and include such aspects as the insurance mandate on most U.S. citizens as well as some of the key points the act will implement.
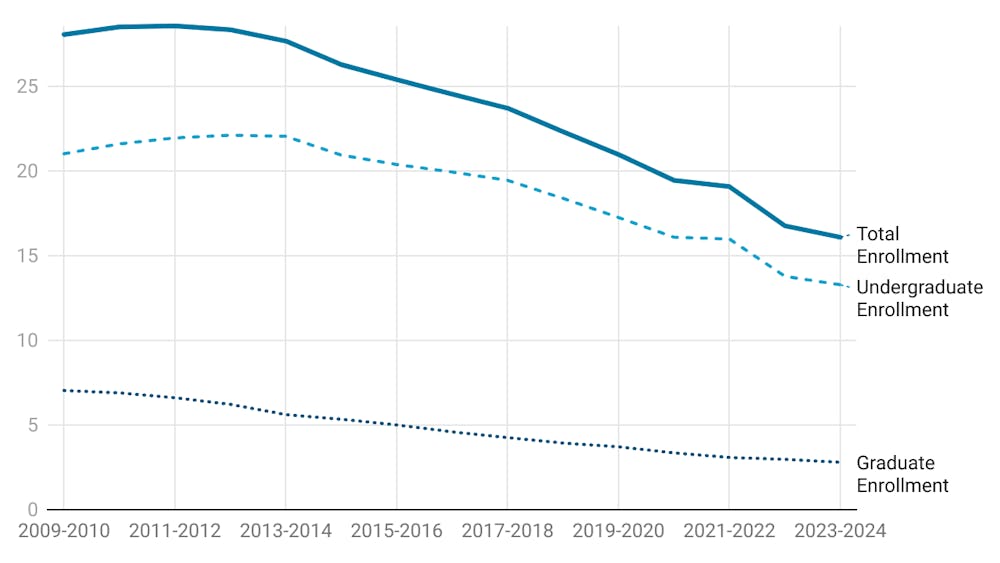
“Exploring Trends in Gerontology Higher Education in the United States” by Andrea Gossett Zakrajsek discussed the evolving trends in higher education programs in both the U.S. and EMU. Zakrajsek is the director of the Aging Studies program at EMU. Formal Gerontology instruction began in the U.S after the passing of the Older Americans Act in 1965.
Currently, there are 750 programs in more than 500 schools across the U.S., including EMU’s program, which was initiated in 1976. Though gerontology does not have its own degree yet, there is a growing need for professionals in the field and predictions expect that with the “baby boom” generation soon to reach older ages, the need for those with certification in this field will steadily increase by the year 2030.
EMU students were in attendance in addition to the medical personnel participating through Microsoft Link. Muneez Patel was one of many students in attendance for the conference.
“I might focus on geriatric care because I’m going to be a graduate student in health education in the future,” Patel said, who is currently a senior. He will graduate this upcoming winter semester and will be completing his graduate studies at EMU as well.
This event was approved for LBC credit.